The course of the disease
Our editors will review what you’ve submitted and determine whether to revise the article.
- Center for Disease Control and Prevention - Smallpox
- National Center for Biotechnology Information - Smallpox
- The Nemours Foundation - For Teens - Smallpox
- Healthline - Smallpox
- WebMD - Smallpox
- MSD Manual - Professional Version - Smallpox
- Mayo Clinic - Small Pox
- DermNet - Smallpox
- Biology LibreTexts - Smallpox
- eMedicineHealth - Smallpox
- Cleveland Clinic - Smallpox
- Also called:
- variola major
News •
Each case of smallpox arose from close contact with another case of the disease, usually by inhalation of virus that had been expelled in the breath or saliva droplets of an infected person. Despite the hardiness of the variola virus, smallpox was not a highly infectious disease; infected persons usually did not infect more than two to five of their closest contacts. The great danger from the disease was that it could cause only a very mild attack in vaccinated persons, yet these persons could unwittingly spread the fatal form of the disease. It was therefore essential in dealing with an outbreak to make thorough enquiry into all possible contacts of patients and to follow these contacts and either ascertain that they had escaped infection or else isolate them at once if they showed any sign of infection.
Once variola major entered the body through the mucous membranes of the respiratory tract, there was a one- to two-week incubation period during which the person showed no signs of infection. The virus multiplied in the lymph nodes, spleen, and bone marrow, then migrated in white blood cells to small blood vessels near the surface of the skin. Illness first became apparent with a sudden high fever of 38.5 to 40.5 °C (101 to 105 °F), severe headache and back pain, and sometimes abdominal pain and vomiting. Two to five days later these flulike symptoms abated. However, they were followed by the appearance of lesions in the mouth and by a rash on the skin that was heaviest on the face and lower part of the limbs, displaying what was called a centrifugal, or centre-fleeing, distribution. The rash might be so profuse as to be confluent, especially on the face, or so scanty that the lesions were missed altogether. The first manifestation of the rash was a flat spot, or macule, which over the next few days changed into a raised papule, then into a clear blister, or vesicle, and finally into an infected pustule. By this time the fever usually returned. In fatal cases, death frequently came after a week or two of illness, brought on by the toxic effects of huge quantities of virus in the blood and the inflammatory response of the body’s immune system. In nonfatal cases, the pustules dried up and formed scabs that, upon separation, left multiple pockmarked scars.
In some cases there was a toxic eruption during the initial fever, before the appearance of the true smallpox rash. These toxic rashes might be diffuse blushes on trunk or limbs, somewhat suggestive of scarlet fever or measles; they might, on the other hand, be deeper red, with small hemorrhages like fleabites or larger blotches in the skin. The first type of rash was clinically unimportant, but the deep red, hemorrhagic rash occurred in the most severe, usually fatal cases of the disease. Frequently such patients died before the true smallpox rash had time to develop, and the disease was not diagnosed. These cases were not usually sources of infection, however, because smallpox was not infectious until the characteristic focal eruption had come out in the throat and on the skin.
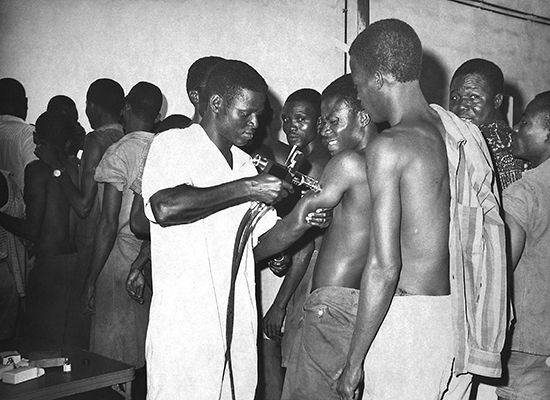
If smallpox vaccine was given within a few days of exposure to the virus, it would act to prevent illness or lessen the degree of symptoms. However, once symptoms appeared, treatment was limited. The patient was kept as clean and comfortable as possible, the fever was treated with analgesics, and pustules were treated with antiseptics to prevent secondary infection.
The Editors of Encyclopaedia Britannica